Measles Cases Surge Worldwide: A Deep Dive into the Resurgence of an Eliminated Disease







2025-05-12T04:18:46Z
Measles is making a troubling comeback globally, with significant increases in reported cases across the United States, Canada, Mexico, South America, and parts of Europe. In a stark contrast to previous years, North and South America collectively reported eleven times more cases in the first quarter of 2025 compared to the same period in the previous year. Meanwhile, Europe is seeing rates that are unprecedented in the last 25 years, indicating a widespread resurgence of this highly contagious disease.
As of May 2, 2025, health authorities in the United States confirmed a staggering 935 measles cases across 30 states, marking a significant spike from the 285 cases documented in 2024. In Canada, the situation is equally alarming, with reports exceeding 1,000 cases, primarily attributed to an ongoing outbreak.
To understand the implications of this surge, The Conversation reached out to Rebecca Schein, a specialist in pediatric infectious diseases. Schein provided insights into how the current measles statistics compare to historical data and what it might mean for public health.
Historically, the U.S. saw fewer than 100 measles cases annually from 2000 to 2010. This changed in the following decade, as isolated outbreaks primarily affected unvaccinated communities, with cases averaging between 200 and 300 each year. The last significant outbreak before the recent surge occurred in 2019, when 1,274 cases were reported, predominantly in the New York City metropolitan area and nearby New Jersey.
The COVID-19 pandemic temporarily reduced measles cases between 2020 and 2023, but by 2024, numbers returned to pre-pandemic levels. Currently, Texas is the epicenter of the outbreak, with 702 confirmed cases as of May 6, 2025. Tragically, this outbreak has resulted in 91 hospitalizations and three deaths, including two children.
The World Health Organization (WHO) has raised alarms, declaring both North and South America to be at high risk for measles. Canada reported a total of 1,177 cases as of April 19, with 951 linked to an outbreak that began in New Brunswick in October 2024 and extended to seven provinces. In stark contrast, Canada recorded only 12 measles cases total in 2023.
In Mexico, the situation is also concerning, with 421 confirmed measles cases reported as of April 18 and an additional 384 cases currently under investigation. Other South American countries are experiencing small outbreaks as well, with Belize confirming its first two cases since 1991, Brazil reporting five cases, and Argentina noting 21 confirmed cases, primarily in Buenos Aires.
Europe has not been spared from this resurgence, witnessing a tenfold increase in measles cases with a total of 35,212 reported in 2024, according to the European Centre for Disease Prevention and Control. This alarming trend highlights the potential for measles to spread widely if vaccination rates do not improve.
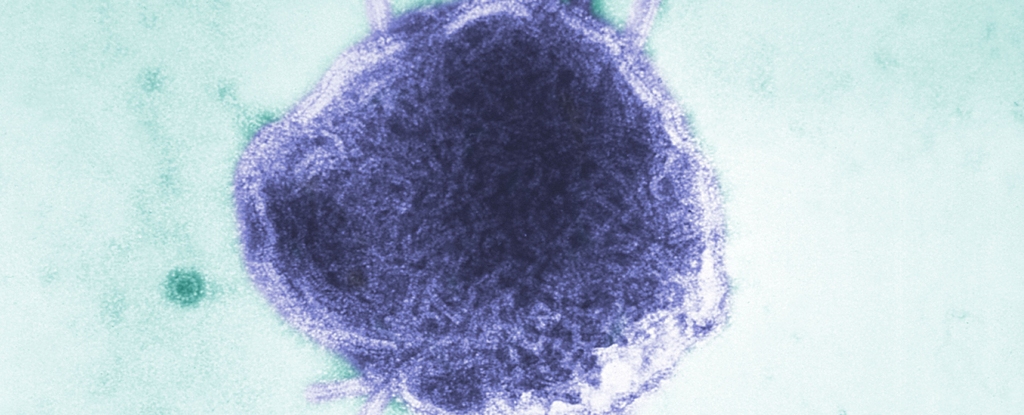
Measles is one of the most contagious diseases known, with an infected person capable of transmitting the virus to 12 to 18 others. This high contagion rate is often compared to the flu, which has an R0 of 1 to 4, and COVID-19, which ranges from 2 to 5.
The history of measles in the United States dates back to 1912, when it became a nationally reportable disease, with approximately 3 million to 4 million cases and about 6,000 deaths each year. Although medical advancements gradually decreased the death rate, the disease would still reach epidemic levels every few years. The introduction of the first measles vaccine in 1963 dramatically changed this trend. The current MMR vaccine, which protects against measles, mumps, and rubella, was introduced in 1971.
In 1977, the U.S. government implemented the National Childhood Immunization Initiative, mandating vaccinations against several diseases, including measles. By 1981, childhood vaccination rates soared to 96%. Programs like Vaccines for Children, initiated in 1993, aimed to provide access to vaccinations for all children, irrespective of financial circumstances. These efforts resulted in the elimination of measles in the U.S. by the year 2000, as cases were predominantly linked to international travelers.
The current rise in measles cases raises significant concerns for public health. Vaccination helps the body develop antibodies to combat specific infections, and most individuals are protected from measles with just one dose of the vaccine. The second dose serves to enhance long-term immunity. For a community to achieve herd immunity—where enough people are vaccinated to protect those who cannot be vaccinated—approximately 95% of the population must be immunized.
Over the past two decades, however, global vaccination rates have been declining, a trend exacerbated by the COVID-19 pandemic, which limited access to healthcare services and routine immunizations. As vaccination rates wane, infectious disease experts express grave concerns that measles could once again become a common illness in the United States.
If this trend continues unchecked, public health officials warn that the U.S. could see a return to endemic measles. A 2022 study utilized a computer model to project the trajectory of measles cases in the U.S. and found that if the current decline in vaccination rates persists, approximately 15 million children—21% of U.S. children—could be vulnerable to measles within the next five years. This situation poses a significant risk for future outbreaks.
Another model published in April 2025 suggested that if vaccination rates do not improve, the U.S. could face up to 850,000 measles cases over the next 25 years. Should vaccine uptake decline further, projections indicate that this number could soar to 11 million cases in the same timeframe.
To reverse this concerning trend, increased vaccination rates are crucial. The April 2025 study indicated that even a modest increase of 5% in community vaccination rates could reduce potential cases to between 3,000 and 19,000 over the next 25 years.
Another epidemiological study from February highlighted the importance of early intervention during measles outbreaks. The research suggests that if local health departments act promptly, containing outbreaks is feasible as long as at least 85% of the population is vaccinated. Achieving this level of immunity requires not only access to affordable vaccinations but also building and restoring public confidence in measles vaccines.
As we reflect on the rise of measles cases globally, the insights from experts like Rebecca Schein underscore the pressing need for renewed commitment to vaccination programs and public health initiatives to safeguard against the resurgence of this preventable disease.
This article has been republished from The Conversation under a Creative Commons license. For the original article, please visit their website.
 Isabelle Moreau
Isabelle Moreau
Source of the news: ScienceAlert